Comprehensive Management of Dizziness in Elderly Clients
Sandra M. Nettina, MSN, RN, CS, ANP
© 2001 Medscape, Inc.]
Abstract
Dizziness is a symptom experienced by one
quarter to one third of older adults. Etiology includes a variety of central
nervous system, cardiovascular, otologic, and sensory causes. One of the most
common causes is benign positional vertigo, a peripheral vestibular
dysfunction. Although benign positional vertigo and many other causes are not
life threatening, dizziness from any cause can negatively affect the client's
life and cause injury. Since the cause of dizziness may be difficult to
diagnose, nursing management should focus on the impact of dizziness. Treatment
strategies should include frequent monitoring to improve overall health or to
deal with other conditions that may contribute to dizziness, safety measures to
prevent falls, patient education about antivertiginous medications, and
referral for vestibular rehabilitation. The advanced practice nurse (APN) plays
a significant role in the assessment of dizziness and the reduction of its
impact on the elderly client.
Case Study
Mrs. Smith is a 72-year-old woman residing
in an assisted living facility who complains of intermittent, daily episodes of
dizziness, usually while arising from bed. The episodes last several hours and
diminish in the early afternoon. She notes that the room spins and the feeling
is exacerbated by turning her head. Past medical history is significant for
myocardial infarction, mild heart failure, atrial fibrillation, and
hypothyroidism. Medications include atenolol 100 mg daily, verapamil 180 mg
daily, furosemide 20 mg daily, levothyroxine 0.1 mg daily, coumadin 5 mg daily,
and docusate 100 mg daily. She told her doctor about the dizziness, and was
prescribed meclizine 25 mg 3 times a day as needed, with only minor relief.
Mrs. Smith takes her meals in the dining room but often skips breakfast for
fear of falling on her way. She is worried about going to her niece's home for
a family party next week.
Introduction
Dizziness is a common symptom in people of
all ages, particularly the older adult. Dizziness is a generic term used to describe
a variety of experiences including giddiness, lightheadedness, faintness,
vertigo, fogginess, imbalance, unsteadiness, and ataxia. The etiology of a
person's complaint of dizziness is often difficult to identify. Origins include
problems of the inner ear and vestibular branch of the eighth cranial nerve,
cerebrovascular insufficiency and other problems of the central nervous system,
cardiovascular dysfunction, metabolic disorders, sensory deficits, and
emotional disorders (Table 1). A combination of causes occurs in many cases.
Older adults may accept dizziness as a symptom of aging without
seeking treatment. Others may become alarmed, associating dizziness with
life-threatening stroke or cardiovascular disease. Despite the etiology,
however, dizziness represents a significant hardship for many older adults.
Despite appropriate medical work up and interventions, the person's life might
continue to be greatly affected by dizziness. In many cases, the diagnosis is
not identified, or dizziness persists despite diagnosis and treatment. Quality
of life may be impaired, and falls and other injuries may result.
The APN can play an instrumental role in the management of
dizziness. The APN can help the person adapt to dizziness, ensure safety, and
even help alleviate the symptoms of dizziness. While the medical team of
specialists will focus on differentiating the underlying cause, the APN can
take a more patient-centered and holistic approach.
Scope of the Problem
Studies have shown that approximately one
quarter to one third of elderly in the community are dizzy.[1,2] One study showed that 1 in 10
respondents suffered from current, handicapping dizziness.[3] Many patients report dizziness to their
primary care provider (PCP), and 5% to 10% of new primary care visits are for
dizziness.[4]
The differential diagnosis of dizziness often presents a dilemma
to the PCP. Most people presenting with dizziness will have a normal physical
examination despite significant, often life-altering and debilitating,
symptoms. Laboratory testing and imaging studies usually prove worthless in
determining the diagnosis of dizziness.[5] The PCP often tries to narrow the
differential diagnosis by symptomatology to determine the appropriate referral.
Patients are more likely to be referred to a specialist if symptoms last 1 year
or longer, there is more than 1 visit to the PCP for dizziness, and there are
additional symptoms pointing to a cardiac; neurologic; or ear, nose, or throat
disorder.[6] Some researchers have set out to show that patients with
dizziness are underreferred[6] and that most cases of unexplained dizziness can be
diagnosed if work up is sufficiently extensive.[7,8] In fact, numerous studies have been done
to find out the diagnostic breakdown of dizziness in the elderly and to
determine predictors of certain causes that might assist in better evaluation
and referral criteria.[7-10] However, little outcome research has
been done to show improved quality of life or decreased morbidity and mortality
with aggressive evaluation and treatment for the vast differential of
dizziness.
Work by Tinetti and colleagues[11] takes a different approach to dizziness.
They have proposed that dizziness should be treated as a geriatric syndrome
rather than a symptom of an underlying disorder. They found that chronic
dizziness was not associated with increased mortality or hospitalizations.[11] They did find that dizziness was
associated with worsening of some quality-of-life indicators, as have other
studies,[2] as well as with risk of falling and depression. Falls or
fear of falling may be the greatest threat with dizziness. Burker and
colleagues[12] found that 47% of the elderly who are dizzy have a fear of
falling, as opposed to 3% of controls. Von Renteln-Kruse and colleagues[13] reported that elderly patients with
dizziness were 10 times more likely to report falls than those without
dizziness. Tinetti and colleagues[1] suggested that impairment reduction strategies might prove
more effective in reducing the disability of dizziness than focusing on
identifying and treating particular causes.
Screening and Assessment
Screening
Psychogenic dizziness is often listed as
an etiology of the complaint of dizziness. This seems to be a diagnosis of
exclusion when no other etiology can be found and the patient suffers from
anxiety, depression, or some other emotional malady. Many studies have shown a
correlation of dizziness to anxiety and depression, but have not proven a cause
and effect relationship.[2,14] Dizziness should be regarded as a
significant symptom with important impact on an elderly individual's well
being, and, therefore, all elderly people should be regularly screened for the
symptom of dizziness, especially those who also have anxiety and depression.
Likewise, a person who has complained of dizziness should also be screened for
emotional effects, including anxiety and depression.
General History
The approach to the patient with dizziness
should begin with an assessment of the complaint. Many patients will have
complained to their PCP of dizziness in the past. They may have seen
specialists, had diagnostic testing, and been told that it was nothing serious.
Antivertiginous medication such as meclizine may have been prescribed but may
not have worked, or the patient might have believed it wasn't worth taking.
This scenario is not a reason to stop the data gathering about
dizziness; rather, it is the perfect opportunity to explore the impact of
dizziness on the patient's life. Standard assessment parameters should be
explored, such as type of sensation experienced, frequency, duration,
intensity, precipitating and alleviating factors, and associated symptoms.
History findings may point to the etiology of dizziness, but, more importantly,
show areas for further evaluation, the impact of dizziness on the person, and
areas for intervention.
A number of patients have more than 1 sensation of dizziness.[1] A spinning sensation without
lightheadedness is more likely related to benign positional vertigo.[14] Syncope is often associated with
cardiovascular disorder.[9,10] Many patients -- but not all -- with
benign positional vertigo will report dizziness precipitated by position
change.[15]
Associated symptoms may be subtle and not previously reported by
the patient. Therefore, review of systems should be broad and include questions
about such things as general health, headache, visual or hearing problems,
tinnitus, signs of peripheral neuropathy, arthritis, neck pain, shortness of
breath and hyperventilation, palpitations, and nausea and vomiting.
Medication History
The patient's current and recent
medications should be evaluated. Use of aminoglycoside antibiotics may cause
ototoxicity, as can the loop diuretic ethacrynic acid. Use of any diuretics may
be associated with volume depletion, leading to lightheadedness.
Antihypertensives and vasodilators may cause postural lightheadedness.[16] Antihistamines, anticholinergic agents,
antidepressants, antianxiety agents, nonsteroidal anti-inflammatory drugs, and
just about any drug that works through the central nervous system may cause
dizziness in some people. A study of hospitalized patients ages 75 years and
older found that neuroleptics, antidepressants, hypnotics/sedatives, and
combinations of drugs with hypotensive effects were prescribed more frequently
in patients who reported dizziness.[13]
Some research has focused on the number of medications taken by
the elderly as being a factor in dizziness and falls. However, Hendrich and
colleagues[17] found that the presence of medication side effects was a
better predictor of falls than the medications themselves. Therefore,
medication history should include questioning about potential medication side
effects such as sedation, impaired balance, and dizziness.
Additionally, medications used to reduce dizziness should be
reviewed. Although meclizine and a few other antivertiginous agents are
approved for the treatment of vestibular-related dizziness, they may actually
cause or exacerbate dizziness. Paradoxic effects such as restlessness,
irritability, insomnia, euphoria, auditory and visual hallucinations, and
diplopia may occur in the elderly.[18] Antivertiginous medications are more effective for motion
sickness and acute labyrinthitis rather than benign positional vertigo and
other causes.[18,19] Therefore, if positive results are not
seen, these agents should be discontinued.
General Physical Examination
Physical examination should follow
history. If a thorough neurologic exam was done and no focal deficits were
documented, then it need not be repeated. However, there are several areas on
which the APN should focus. If the history reveals possible sensory deficits,
then vision, hearing, proprioception, light touch, and vibratory sensation
should be evaluated thoroughly. Dysequilibrium or other sensations of dizziness
may arise from multiple sensory deficits. Otoscopic assessment of the ears
should be conducted to screen for impacted cerumen or infection, which may
contribute to dizziness. A cardiovascular exam should include assessment for
vital signs, orthostatic blood pressure changes, carotid bruits, and
auscultation of the heart for rate, rhythm, and murmur. A new arrhythmia or
valvular dysfunction may contribute to dizziness.
Orthostatic changes. Physical assessment of the dizzy patient
should also focus on postural blood pressure changes. Orthostatic hypotension
occurs more commonly in the elderly and may be related to such conditions as
cardiovascular disorders, Parkinson's disease, or medication side effects.
Results of studies on the relationship between postural hypotension and
dizziness have varied based on varying parameters used to define orthostatic
changes.[1,20] Orthostatic hypotension is frequently defined as a drop in
systolic blood pressure of 20 mm on position change from supine to standing;
however, many studies have found more modest changes that relate to dizziness.
Hillen and colleagues[21] found that systolic decrease of 15 mm Hg and diastolic
decrease of 5 mm Hg related to dizziness. Tinetti and colleagues[1] found a relation only between mean blood
pressure change and dizziness, possibly because mean blood pressure correlates
better with cerebral perfusion.
In any case, blood pressure and pulse responses to position change
should be assessed immediately and at 2 minutes to screen for orthostatic
hypotension that may be related to dizziness. The patient should also be
observed for clinical signs and symptoms such as nausea, pallor, dizziness,
visual dimming, and decreased consciousness in assessing orthostasis.[22]
Dix-Hallpike maneuver. Provocation tests for dizziness often
identify dizziness of a vestibular nature and thus rule out the need for a more
thorough cardiac work up. The Dix-Hallpike maneuver (also called the Nylen
maneuver, Barany maneuver, or drop test) should be performed on all patients
complaining of dizziness. It can be done on an examination table or in the
patient's bed, provided there is room for the patient's head to hang over the
edge of the bed. The procedure should be explained to the patient thoroughly
prior to the maneuver (Table 2).
The Dix-Hallpike is diagnostic for benign positional vertigo when
dizziness is reproduced by this maneuver with nystagmus to 1 side that occurs
after a 4-5 second latent period. If nystagmus occurs immediately upon this
maneuver, lasts more than 30 seconds, is exclusively vertical, or is
nonfatiguable with repeated maneuvers, then a serious central nervous system
lesion may be present.[18,23]
In a study[15] of 191 patients referred to a neurology clinic with a
variety of diagnoses and complaints such as unusual sensations of dizziness,
neck pain, and headache, 36 were identified with benign positional vertigo. The
Dix-Hallpike had not been performed on any of these patients prior to referral.
The authors concluded that the Dix-Hallpike is mandatory for all patients
complaining of dizziness or vertigo. Had it been performed in the primary care
or long-term care setting, unnecessary work up and referral might have been
avoided.
Management
Treatment of Etiologic Factors
Obviously, etiologic factors for dizziness
should be treated whenever possible. The APN can ensure that identified
cardiovascular disorders are monitored and controlled adequately. The APN should
facilitate additional testing such as electrocardiogram (EKG) and
echocardiogram, and refer to the cardiologist if the patient becomes
symptomatic, has difficulty adhering to the medication regime, or shows signs
of decompensation such as heart failure. For sensory deficits related to
dizziness, the APN can help the patient obtain a hearing aid, visual
correction, and ambulatory aids. The APN can treat impacted cerumen and make
referral for additional ear problems. The APN should make recommendations for
adjustments to the medication regime if dizziness is thought to be a side
effect of 1 or a group of medications.
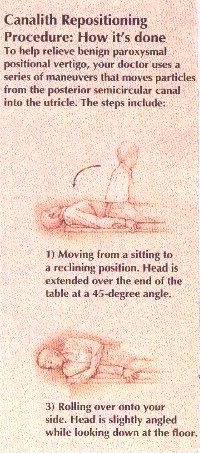
Vestibular Rehabilitation
Vestibular rehabilitation, also known as
vestibular exercises, canalith repositioning maneuver, or the Epley maneuver,
is the one definitive treatment for vestibular causes of dizziness. It can
greatly reduce the symptom of dizziness, but unfortunately is not widely used
in many settings. It may be done by the clinician immediately following a
positive Dix-Hallpike maneuver[23] and often produces a dramatic decrease in dizziness.
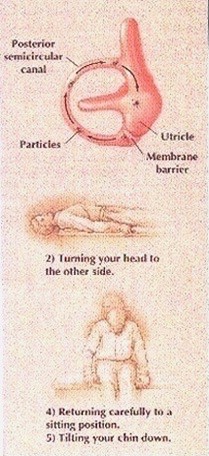
Because benign positional vertigo results from the free movement
of dislodged particulate debris into the posterior semicircular canal,
vestibular rehabilitation acts to reposition the loose particles from the
posterior semicircular canal into the utricle. This is accomplished by
maneuvering the patient's head into certain positions. For patients
with central causes of dizziness, vestibular rehabilitation may also include
gait training and strengthening of other sensory functions to compensate for
vestibular dysfunction.[16] A physical therapist may be consulted in any case.
Vestibular exercises may be performed several times by the therapist, then
taught to the patient to perform at home. Antivertiginous and central nervous
system medications should be avoided during therapy because the sensation of
dizziness is required for effective compensation.[18]
Efficacy of vestibular rehabilitation was retrospectively studied[24] in 37 patients with both peripheral and
central vestibular etiologies of dizziness by comparing dizziness handicap
inventory scores pretreatment and posttreatment within 1 year of vestibular
rehabilitation. A significant improvement in test scores was found
posttreatment. There was no significant difference in improvement between
patients who performed home exercises for at least 1 month and those who
participated in initial therapy only. Gordon and colleagues[15] found complete resolution of dizziness
in 83% of patients diagnosed with benign positional vertigo following 1
physical therapy session. The APN should use this knowledge to facilitate
referral of the patient with chronic dizziness to a physical therapist who
provides vestibular rehabilitation. This is an option that may not have been
considered by the PCP or specialist evaluating the patient in the past.
Antivertiginous Medications
Antivertiginous medications, particularly
meclizine, are prescribed widely for all ages of people who are dizzy. These
agents, however, are most effective for motion sickness and only possibly
effective for vertigo caused by vestibular disorders. These drugs may have
central nervous system depressant effects or paradoxic effects in the elderly.
They have anticholinergic effects so should be avoided with narrow angle
glaucoma, benign prostatic hyperplasia, and gastric and genitourinary outlet
obstruction. Additional anticholinergic side effects, which may be additive
with other anticholinergics, may include xerostomia, blurred vision,
constipation, urinary retention, and mental status changes.
Despite the precautions, meclizine 12.5 mg to 25 mg may be used 2
to 3 times daily to control or prevent dizziness. It works by decreasing
labyrinth excitability and conduction in the vestibular-cerebellar pathways.
Onset of action is 20 minutes to 60 minutes, so meclizine may do little to
treat a vertiginous attack already in progress. Elderly patients should be
cautioned to avoid activities that require mental alertness, such as driving,
until the effects of the medication are fully revealed.
Diphenidol is another antivertiginous and antiemetic medication
that is sometimes used for vertigo associated with nausea and vomiting. It is
not a first-line agent because of its propensity for central nervous system
side effects such as mental status changes, hallucinations, disorientation, and
confusion. Dimenhydrinate is an antihistamine used for motion sickness. It may
cause central nervous system side effects and photosensitivity.
The APN should take an active role in educating patients about
these drugs, their side effects, proper use, and limitations. Care should be
taken to avoid interactions of other drugs with anticholinergic and central
nervous system effects. The APN can monitor drug effectiveness with the patient
and should recommend discontinuing the drug if significant side effects occur
or no benefit is seen.
Ensuring Safety
Safety is a primary concern for the
elderly patient who is dizzy, both to prevent injury and to prevent inactivity
and withdrawal due to fear of falling. There are a number of ways the APN can
intervene to ensure the elderly patient's safety. First, the patient's
immediate environment should be safety-proofed to prevent injury if the patient
becomes dizzy and unsteady. The patient should be encouraged to wear properly
fitting nonslip footwear. Furniture should be removed that has sharp edges or
that may be an obstruction. Throw rugs should be removed, lighting should be
good, and steps should be fully visible with handrails on 2 sides. The patient
should be taught how to arise slowly and avoid sudden position changes if
postural or position changes aggravate dizziness. T'ai Chi may be helpful for
improving balance in people with dizziness and dysequilibrium. Research has
shown significant improvement in people with mild balance disorders.[25]
The topic of driving should be discussed with the dizzy patient.
Although many elderly patients depend on driving for daily functioning, dizziness
poses a potentially lethal threat. In 1 study,[26] few dizzy subjects had been warned by
their doctors not to drive, and 52% said that if they were warned to stop
driving, they would not. Therefore, the topic needs to be approached
sensitively, in an effort to help the patient avoid dependence on driving while
dizzy. Plans should be made for alternate transportation if the patient is
dizzy, and an emergency plan can be made to stop the car in a safe place if
dizziness ensues while driving.
Summary
The APN is in a unique position to
intervene with the elderly client who is dizzy, no matter what the cause. While
the medical work up is progressing, as well as following the diagnosis, the APN
can address the impact of dizziness on the patient. The APN should determine if
a thorough neurologic and cardiovascular examination has been performed. Unless
focal neurologic deficits, severe headache, and vertical nystagmus are present,
neuroimaging is not necessary. The Dix-Hallpike maneuver should be performed on
all dizzy patients to rule out a benign peripheral vestibular etiology for the
dizziness. A positive test indicates the need for vestibular rehabilitation.
The APN should facilitate this referral to a physical therapist and involve the
patient's family and other caregivers to help address issues of fall
prevention, driving safety, and careful use of antivertiginous medications.
Case Study -- Conclusion
The medical record for Mrs. Smith
indicated a normal neurologic examination with negative Romberg test and intact
proprioception, reflexes, and light touch sensation, but the Dix-Hallpike
maneuver had not been performed. Cardiac and audiologic evaluations were
normal. The APN repeated an ear exam, which revealed no abnormalities. The APN
also evaluated for postural hypotension, which was absent, obtained an EKG that
revealed normal sinus rhythm, and performed a Dix-Hallpike maneuver. The
Dix-Hallpike revealed positive horizontal nystagmus toward the left that
disappeared when tried again. This finding with history of intermittent
positional vertigo confirmed a diagnosis of benign positional vertigo. The APN
recommended that Mrs. Smith's meclizine be discontinued since it was not
effective. A referral was made for treatment by a physical therapist for
vestibular rehabilitation. Following 2 treatments, Mrs. Smith's dizziness was
significantly better and she began going to the dining room every morning. The
physical therapist suggested that a cane could be obtained if Mrs. Smith
desired until she became completely steady. Mrs. Smith refused. The APN asked
the staff to make sure that Mrs. Smith wear appropriate footwear at all times,
and to keep her room free from clutter. The APN continued to monitor Mrs.
Smith's cardiac status and coagulation profile and reinforced patient and staff
education to prevent bleeding with anticoagulant use.
Table 1. Differential Diagnosis of Dizziness
|
Character of Dizziness |
Mechanism |
Examples |
|
Lightheadedness, faintness, presyncope |
Vaso-vagal mediated |
Carotid sinus hypersensitivity |
|
Neuromediated |
Volume depletion |
|
|
Autonomic neuropathy of diabetes |
||
|
Severe anemia |
||
|
Aortic stenosis |
||
|
Drugs |
||
|
Metabolic disturbance |
Hypoglycemia |
|
|
Hypoxia |
||
|
Vertigo |
Peripheral vestibular |
Benign positional vertigo |
|
Labyrinthitis |
||
|
Meniere's disease |
||
|
Ototoxic drugs |
||
|
Acoustic neuroma |
||
|
Central vestibular |
Vertebrobasilar insufficiency |
|
|
Multiple sclerosis |
||
|
Drugs in excess |
||
|
Ataxia, dysequilibrium |
Multiple sensory deficits |
Diabetes mellitus |
|
Impaired vision |
||
|
Motor problems |
||
|
Cerebellar disease |
Cerebellar degeneration |
|
|
Cerebellar hemorrhage |
||
|
Ill-defined dizziness, anxiety,
fogginess, malaise |
Psychiatric illness |
Anxiety |
|
Depression |
||
|
Psychosis |
.
Table 2. The Dix-Hallpike Test
|
1. |
With patient sitting on the exam table,
maximally extend the neck (to 45 degrees) and turn the head 45 degrees to one
side. |
|
2. |
Support the patient's upper body and ask
the patient to keep eyes open and look at your forehead. |
|
3. |
Suddenly drop the patient backward with
the head over the edge of the table. |
|
4. |
Observe the patient's eyes for at least
15 seconds for the presence of nystagmus. |
|
5. |
Repeat with the head rotated in the
opposite direction. The side with the down ear that produces nystagmus is the
side with the vestibular lesion. |
References
- Tinetti
ME, Williams CS, Gill TM. Dizziness among older adults: a possible
geriatric syndrome. Ann Intern Med. 2000;132:337-344.
- Grimby
A, Rosenhall U. Health-related quality of life and dizziness in old age.
Gerontology. 1995;41:286-298.
- Yardley
L, Burgneay J, Andersson G, Owen N, Nazareth I, Luxon L. Feasibility and
effectiveness of providing vestibular rehabilitation for dizzy patients in
the community. Clin Otolaryngol. 1998;23:442-448.
- Healthtouch
Online. General information on dizziness. Available at: http://www.healthtouch.com/bin/EContent_HT/hdShowLfts.asp?lftname=NINDS014&cid=HTHLTH.
Accessed April 10, 2001.
- Colledge
NR, Barr-Hamilton RM, Lewis SJ, Sellar RJ, Wilson JA. Evaluation of
investigations to diagnose the cause of dizziness in elderly people: a
community based controlled study. BMJ. 1996;313:788-792.
- Bird JC,
Beynon GJ, Prevost AT, Baguley DM. An analysis of referral patterns for
dizziness in the primary care setting. Br J Gen Pract. 1998;48:1828-1832.
- Bath AP,
Walsh RM, Ranalli P, et al. Experience from a multidisciplinary
"dizzy" clinic. Am J Otol. 2000;21:92-97.
- O'Mahony
D, Foote C. Prospective evaluation of unexplained syncope, dizziness, and
falls among community-dwelling elderly adults. J Gerontol A Biol Sci Med
Sci. 1998;53;M435-M440.
- Lawson
J, Fitzgerald J, Birchall J, Aldren CP, Kenny RA. Diagnosis of geriatric
patients with severe dizziness. J Am Geriatr Soc. 1999;47:12-17.
- Allcock
LM, O'Shea D. Diagnostic yield and development of a neurocardiovascular
investigation unit for older adults in a district hospital. J Gerontol A
Biol Sci Med Sci. 2000;55:M458-M462.
- Tinetti
ME, Williams CS, Gill TM. Health, functional, and psychological outcomes
among older persons with chronic dizziness. J Am Geriatr Soc.
2000;48:417-421.
- Burker
EJ, Wong H, Sloane PD, Mattingly D, Preisser J, Mitchell CM. Predictors of
fear of falling in dizzy and nondizzy elderly. Psychol Aging.
1995;10:104-110.
- Von
Renteln-Kruse W, Micol W, Oster P, Schlierf G. Prescription drugs,
dizziness and accidental falls in hospital patients over 75 years of age.
Z Gerontol Geriatr. 1998;31:286-289.
- Oghalai
JS, Manolidis S, Barth JL, Stewart MG, Jenkins HA. Unrecognized benign
positional vertigo in elderly patients. Otolaryngol Head Neck Surg.
2000;122:630-634.
- Gordon
CR, Aur O, Furas R, Kott E, Gadoth N. Pitfalls in the diagnosis of benign
positional vertigo. Harefuah. 2000;138:1024-1027, 1087.
- Goroll
AH, May LA, Mulley AG. Primary Care Medicine: Office Evaluation and
Management of the Adult Patient. Philadelphia, Pa: Lippincott,
Williams & Wilkins; 2000.
- Hendrich
A, Nyhuis A, Kippenbrock T, Soja ME. Hospital falls: development of a
predictive model for clinical practice. Appl Nurs Res. 1995;8:129-139.
- Cohen H,
Mesad SM. Dizziness, vertigo, and ataxia. In: Primary Care.
Philadelphia, Pa: Lippincott, Williams & Wilkins; 1999.
- Pepper
RM. Dizziness. In: Rakel RE, ed. Saunders Manual of Medical
Practice. Philadelphia, Pa: Saunders; 1996.
- Tilvis
RJ, Hakula SM, Valvanne J, Erkinjuntti T. Postural hypotension and
dizziness in a general aged population: a four-year follow-up of the
Helsinki Aging Study. J Am Geriatr Soc. 1996;44:809-814.
- Hillen
ME, Wagner ML, Sage JI. "Subclinical" orthostatic hypotension is
associated with dizziness in elderly patients with Parkinson disease. Arch
Phys Med Rehabil. 1996;77:710-712.
- Winslow
EH, Lane LE, Woods RJ. Dangling: a review of relevant physiology,
research, and practice. Heart Lung. 1995;24:263-272.
- Orient
JM. Sapira's Art & Science of Bedside Diagnosis. 2nd
ed. Philadelphia, Pa: Lippincott, Williams & Wilkins; 2000.
- Cowand
JL, Wrisley DM, Walker M, Stasnick B, Jacobson JT. Efficacy of vestibular
rehabilitation. Otolaryngol Head Neck Surg. 1998;118:49-54.
- Hain TC,
Fuler L, Weil L, Kotsias J. Effects of T'ai Chi on balance. Arch
Otolaryngol Head Neck Surg. 1999;125:1191-1195.
- Sindwani
R, Parnes LS, Goebel JA, Cass SP. Approach to the vestibular patient and
driving: a patient perspective. Otolaryngol Head Neck Surg.
1999;121:13-17.
Edward E.
Rylander, M.D.
Diplomat American
Board of Family Practice.
Diplomat American
Board of Palliative Medicine.